Perimenopause and menopause are a natural phase of life for every woman, marking the end of her reproductive years. Both are a significant, yet often misunderstood, and come with a range of physical, emotional and hormonal changes for a woman, sometimes starting in their 30s or early 40s.
Every woman’s experience through perimenopause and menopause is unique, and the world of hormone levels and hot flashes can be confusing. Oftentimes information available to deal with the intricacies of menopause can be contradictory. However, we believe there are five key things that every woman needs to know about approaching this life-changing event that can help navigate the phase confidently.
1. What is Perimenopause and Menopause?
When it comes to understanding the stages of menopause, the first thing to know is that it is not a sudden event. It is a gradual process and includes several stages that vary from woman to woman.
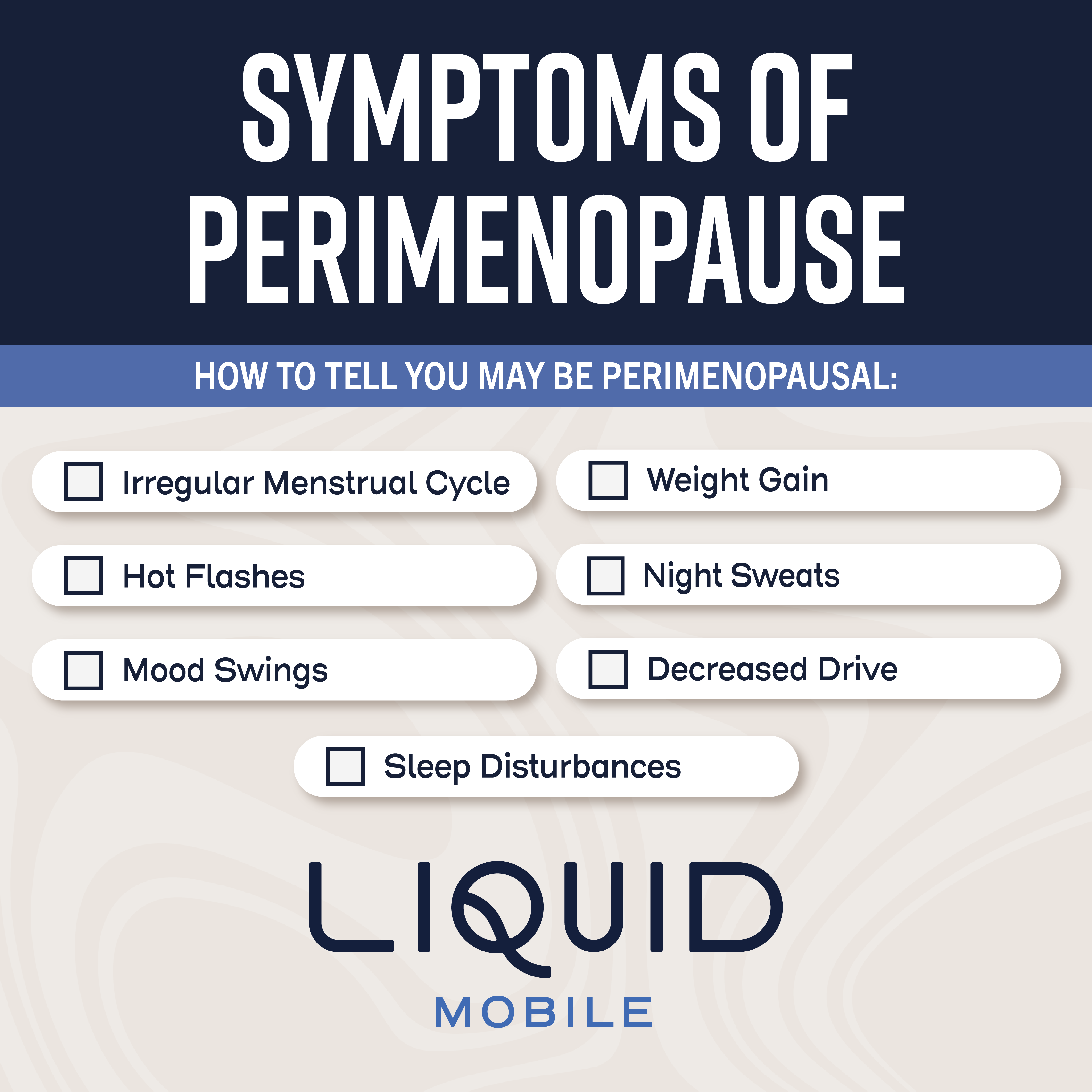
Perimenopause, the phase leading up to menopause, can start while a woman is in her late 30s or early 40s. During perimenopause, hormone levels like estrogen and progesterone begin to fluctuate, which can cause irregular menstrual cycles and other symptoms, including hot flashes, mood swings and sleep disturbances.
A woman is considered to be in menopause when she has not had a menstrual period for 12 consecutive months. Following menopause, a woman then enters post menopause, when most of the symptoms of perimenopause and menopause tend to subside. However, long-term health considerations become even more crucial in post menopause.
2. You can manage your perimenopausal symptoms and menopausal symptoms
The physical and emotional toll that perimenopause and menopause can bring varies greatly among women. However, common symptoms may include hot flashes, night sweats, vaginal dryness, mood swings, hair loss, weight gain, fatigue, diminished mental clarity, sleepless nights and changes in libido. Those symptoms can also differ significantly in severity and duration, but there are ways we can help manage them.
Lifestyle changes, like maintaining a healthy diet, regular exercise and reducing stress through different techniques can certainly help alleviate some of the symptoms.
Additionally, hormone replacement therapy (HRT) and other non-hormonal medications are available options. It is essential that you discuss these options with a healthcare provider, like our clinical expert at Liquid Mobile, to ensure you are receiving the right, and best, plan for you.
3. Menopause and perimenopause can impact bone health
Osteoporosis is a serious risk for women going through these life changes. During menopause, a woman’s estrogen levels drop, which can then lead to a decrease in her bone density. The risk for osteoporosis, the condition where bones become brittle and fragile, increases greatly.
In addition, osteopenia, a condition characterized by lower-than-normal bone density, becomes a pertinent concern during this phase of life. Often considered a precursor to osteoporosis, osteopenia is a condition where bones become extremely fragile and prone to fractures. In osteopenia, bone density is lower than normal but not to the extent seen in osteoporosis. However, the risk of fractures is still heightened, making it a critical concern for women going through menopause.
To maintain bone health, women must ensure they are getting an adequate amount of calcium and vitamin D through diet or supplements, engage in weight-bearing exercises, and take bone health medications to offset the risk.
Regular bone density screenings can also help monitor your bone health and catch any issues early. For some women, lifestyle changes may not be sufficient, and medical interventions may be necessary. Hormone Replacement Therapy (HRT) is a common approach to address the decline in estrogen levels.
Additionally, perimenopause and menopause can lead to Sarcopenia, a loss of muscle mass and strength. Most women can relate to this feeling of muscle loss. They may feel a new jiggle in their triceps, or struggle to get up unassisted. In fact, many people end up in nursing homes due to Sarcopenia, because that loss of muscle and strength leads to a cane, walker, wheelchair and assistance always being needed.
4. Perimenopause and menopause can impact heart health
Heart disease is the leading cause of death among women, and the risk increases after menopause. Estrogen can play a huge role in protecting the heart’s blood vessels. When estrogen levels drop, the risk of heart disease rises.
It is critical that women maintain a heart-healthy lifestyle, including eating a balanced diet, staying physically active and monitoring cholesterol and blood pressure levels. Regular check-ups with a healthcare provider can help assess your heart health, identifying any necessary interventions.
5. Perimenopause and menopause can impact emotional well-being
The hormonal changes associated with the stages of menopause can take a toll on a woman’s emotional well-being. Many women experience mood swings, irritability, anxiety and even depression during this time.
Prioritizing self-care, women should seek support when they feel they need it. This may include talking to a therapist or counselor, practicing relaxation techniques and staying connected with the people in your life you care about most.
Perimenopause and menopause are a natural and inevitable phase of every woman’s life. While it certainly brings various challenges, it can also be an opportunity for growth, self-discovery and positive change. Understanding the stages of menopause and how to manage symptoms, prioritize health and care for your emotional well-being are key to navigating this transition with grace and confidence.
We Can Help
Liquid Mobile utilizes the Brite HRT method of hormone replacement therapy, developed by Dr. Daved Rosensweet. Each Liquid Mobile clinician is trained and certified to provide these services.
Contact us today to speak with an expert clinician, schedule a consultation or have a nurse come to you to talk about HRT and whether or not an HRT plan is right for you. We can help you develop a customized HRT plan to help you feel better.